If you’re an athlete or soldier, or anyone vulnerable to a head injury, you’ve asked the question.
That’s because concussions are a type of non-penetrating traumatic brain injury (TBI), and it’s not known how many can lead to debilitating later-in-life health consequences such as chronic traumatic encephalopathy (CTE).
CTE is a devastating degenerative brain disease found in some athletes, soldiers, and others with a history of repetitive brain trauma.
The prevailing thought has been that TBIs elicit the same physiological response across the population—that most people are similarly affected by one or more head injuries and the best–and really only—response to a TBI is to limit exposure.
It turns out, though, that asking how many concussions is too many isn’t the right question to ask, because it may not be the right way to think about how and to whom TBIs cause damage.
According to research by Steven Kornguth, the right questions have to do with vulnerability versus resilience, and protection versus overcoming.
For some people, one or more TBIs can have devastating effects later in life. For others, whether they’ve had a few or many, there are limited long-term consequences. Because TBIs are experienced differently by different people, there are more relevant ways for you to think about TBI:
- What’s your vulnerability to TBI to and what’s your level of resilience?
- What’s the level of protection you need from a TBI and how can you can overcome its effects once you’ve had one?
“TBI affects people in the prime of their lives. How do we change that? How do we help them? That’s a big motivation for me,” Kornguth says.
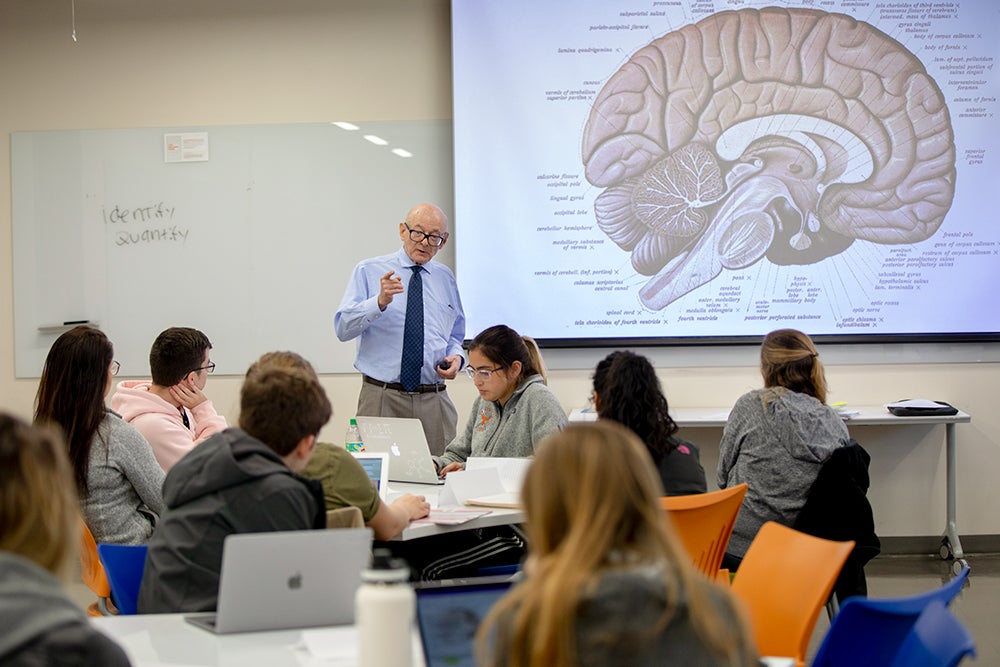
Steven Kornguth teaches “Autoimmune Disease,” an undergraduate course in the College of Education, cross-listed in Undergraduate Studies. The course is open to undergraduates from across the university.
Kornguth is looking at the surprising role of the body’s autoimmune system in TBI development. He is a senior research fellow in the Department of Kinesiology and Health Education and professor of neurology at Dell Medical School.
There are molecular, cellular, and systemic responses to traumatic head and body events, so he and his colleagues are asking a new and surprising question: What is the body’s autoimmune response to TBIs?
Rather than simply looking at limiting exposure to concussions, Kornguth is looking at those who may have high resilience and would be unlikely to suffer long-term consequences, and then what role the autoimmune response plays in that.
Is there an evolving autoimmune process that leads to CTE? If that’s the case, can customized treatment protocols be applied for the management of the autoimmune disease process? Can better and more specialized equipment be provided?
These questions are leading them in an attempt to determine if there are pharmacological treatments that can be offered to reduce the effects of TBI and prevent the development of CTE.
If researchers can understand the level of vulnerability an individual may have in the first place, it’s possible there can be medications given to vulnerable populations before and/or after a TBI that will limit autoimmune response.

Kornguth is one of the nation’s foremost researchers on the long-term effects of concussions on athletes and soldiers. For years, he has worked on biodefense programs with colleagues at the University of Wisconsin Madison, the University of Texas at Austin, and the Army Research Laboratories and Defense Advanced Research Projects Agency in Washington, D.C.
But each spring of the academic year, you can find him leading an undergraduate signature course, Autoimmune Disease, talking about sense-making and the autoimmune system with 18-22 year-olds.
Why does Kornguth choose to teach undergrads? “Why wouldn’t I?” he says. “The rate of scientific discovery relating to the cause and treatment of these diseases is progressing very rapidly, and so as both a faculty member and student, I find there is a new insight we all perceive from each day’s discussion,” he says.
How he does it
Sense-making is one element of Kornguth’s life work. It’s the process of finding patterns in seemingly unrelated data to gain new insight for civilian and soldier protection.
Sense-making is critical in medicine, he says, “where a practitioner can take what appear to be dispersed signs and symptoms reported by a patient, and align these into a fused diagnosis.”
This same process, he notes, is critical in technology innovation and intelligence-gathering, and many other aspects of life in the world.

